In 2024, there are still many interconnected problems facing the global health system, which have been made worse by the COVID-19 pandemic. While the effects of climate change are changing our daily lives more and more, antimicrobial resistance remains a serious threat. Complicating the global health crisis are the reappearance of diseases that were thought to be eradicated, the increasing prevalence of non-communicable diseases, and the glaring disparities in access to healthcare.
In order to address these problems and heal a world confronting never-before-seen challenges, a comprehensive, coordinated response is needed that goes beyond band-aid fixes. This article examines the top 10 global health challenges of 2024, highlighting their interconnectedness, devastating consequences, and the potential for innovative and collaborative solutions.
10 Major Global Health Challenges in 2024
1. Antimicrobial Resistance (AMR)
The threat of antimicrobial resistance is growing. By 2050, it may rise to take up to one in every 27 deaths around the world and even cost the economy of the world up to $ 100 trillion. Resistant bacteria put at risk modern medicine and life-saving procedures dependent on antibiotics: organ transplantation, chemotherapy, and surgery are under threat.
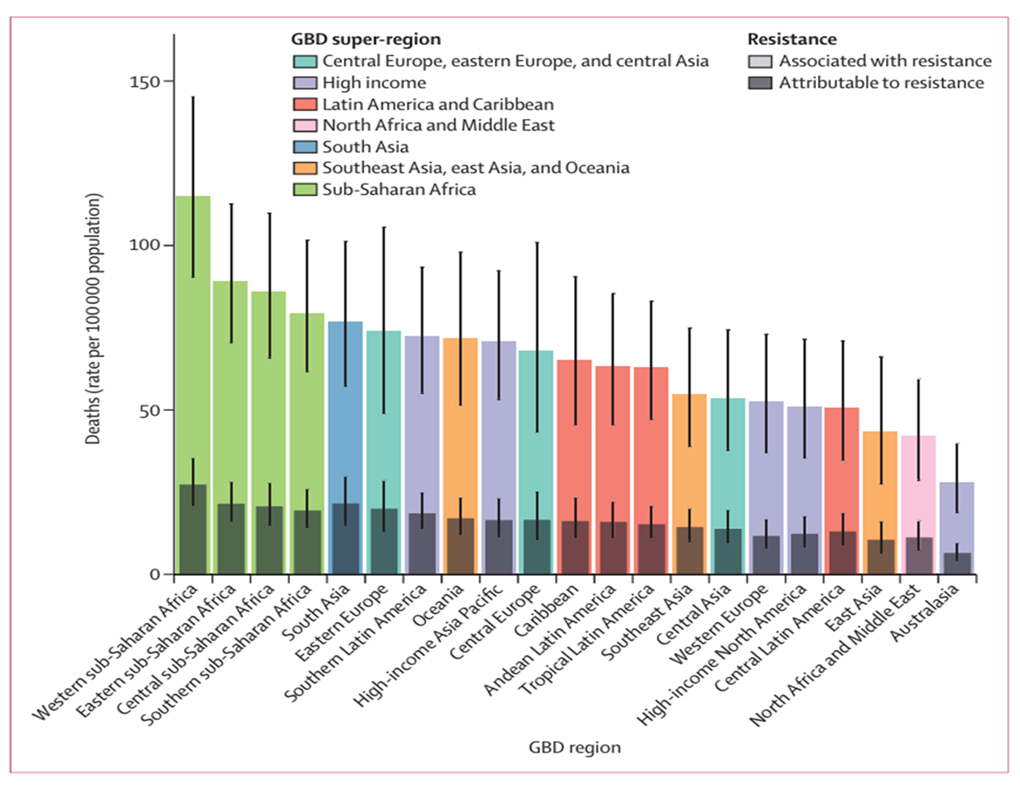
The core drivers of AMR include the overuse and inappropriate use of antibiotics in aquaculture, agriculture, and human medicine. A study published in The Lancet in 2022 provided critical estimates of the impact of bacterial antimicrobial resistance (AMR) across the globe in 2019. The study examined 23 pathogens and 88 pathogen-drug combinations across 204 countries and territories, drawing from data sources including systematic literature reviews, hospital systems, and surveillance networks. In total, 471 million individual records of isolates were analyzed, covering 7,585 study-location-years.
Based on predictive statistical models, the study estimated that bacterial AMR was associated with approximately 4.95 million deaths (95% UI: 3.62–6.57 million), of which 1.27 million deaths (95% UI: 0.911–1.71 million) were directly attributable to bacterial AMR. Regionally, the all-age death rate attributable to AMR was found to be highest in western sub-Saharan Africa, with 27.3 deaths per 100,000 people (95% UI: 20.9–35.3), and lowest in Australasia, with 6.5 deaths per 100,000 people (95% UI: 4.3–9.4). See Fig 1
The WHO has identified that AMR is a high priority and requires immediate, coordinated global action. One of the most important tactics is speeding up the development of new antibiotics—a process hindered thus far by financial, legal, and scientific obstacles. Strengthening surveillance systems, such as the WHO Global Antimicrobial Resistance and Use Surveillance System (GLASS) is essential for monitoring the spread of resistant pathogens and informing public health responses. There is also need to encourage prudent use of the existing antibiotics by putting in place stewardship initiatives within the health system.
2. Climate Change and Health
In regions experiencing more frequent or severe heatwaves, floods, and storms due to climate change, serious health consequences are anticipated. The resultant effect could be physical injuries, waterborne infections, and acute health issues such as heat exhaustion, heatstroke, and the exacerbation of cardiovascular diseases. The long-term health problems are chronic respiratory and cardiovascular conditions and a wide range of mental health disorders, including depression and anxiety. Air pollution, caused by increasing carbon emissions and industrial activities, leads to respiratory disorders such as asthma and COPD.

Climate change influences the distribution and behavior of disease-carrying vectors and has extended the transmission seasons and ranges of diseases like dengue fever and malaria. Such health effects call for a comprehensive approach to mitigation. This needs to focus on carbon emission reduction, transition towards renewable energy sources, increasing energy efficiency, and deploying all forms of sustainable practices. International efforts should focus on building health systems resilient to climate change by strengthening the healthcare system itself, enhancing monitoring and response mechanisms, and adapting health services to altering weather patterns.
3. Non-Communicable Disease
Non-communicable diseases (NCDs) account for 71% percent deaths in the entire world making them a leading cause of death. Of these, 17.9 million annual deaths worldwide are attributed solely to cardiovascular diseases in 2024 estimates. Since many of the NCDs demand long-term medical care and require continuous treatment, they often become highly financially intensive. The rising prevalence of NCDs make a combined method very important. Public health efforts are very important for making people aware of good habits like eating well and exercising regularly, as well as bad habits like smoking and drinking too much.

Changes in lifestyle choices, such as a poor diet, insufficient physical activity, smoking, and excessive alcohol consumption, can significantly reduce the risk of diabetes, cancer, chronic lung conditions, and heart diseases. Putting in place rules that limit dangerous goods and require food labels to include nutritional information can also help to reduce unhealthy eating. Increasing the availability of early diagnosis and treatment is the other key component of NCD treatment. Conditions such as cancer, diabetes, and hypertension all greatly benefit from early diagnosis while also minimising the number of more extensive therapies needed.
There is, therefore, a need to enhance the access level of screening programs of various kinds, provide diagnostic services at cheaper costs, and have access to effective treatment as part of better managing NCDs and reducing their general burden.
4. Infectious Diseases and Pandemic Preparedness
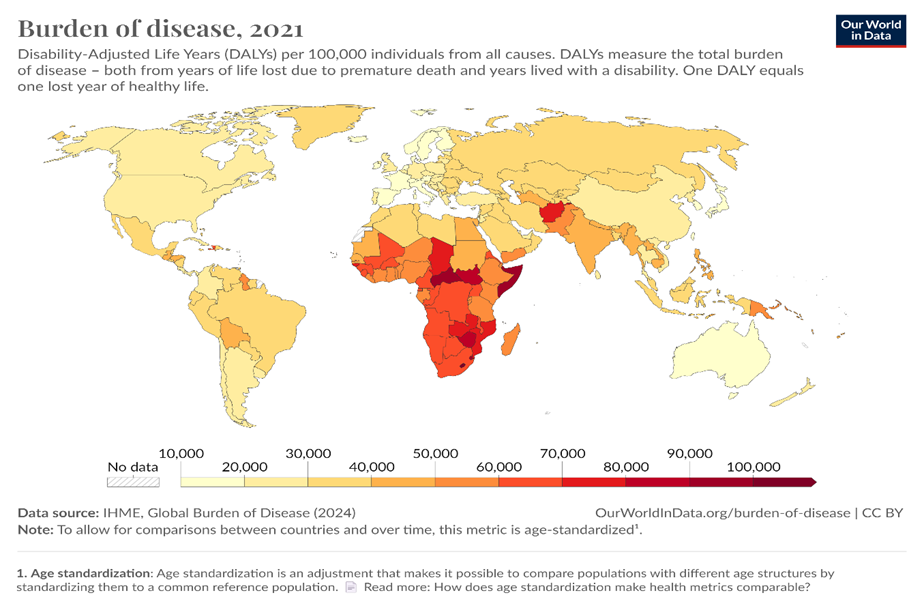
From the image below, we see that even though much has been done to fight infectious illnesses, they remain a continual threat to world health especially in Africa. Claiming nearly 6.9 million deaths worldwide as of 2024, the COVID-19 epidemic has shown the need for strong pandemic preparedness and reaction mechanisms. Infectious diseases such HIV/AIDS, TB, and malaria still cause major morbidity and death in low and middle-income countries. In 2022 alone, over 627,000 deaths from malaria—mostly from sub-Saharan Africa—have been reported. Dealing with these issues calls for investments in research and development, strengthening of world health systems, and guarantee of fair access to vaccines and treatments.
5. Mental Health

In low- and middle-income nations, where mental health treatment services are frequently either nonexistent or insufficient, the most noticeable increase in the prevalence of mental health disorders is seen. Consequently, this leads to the spread of health problems like substance abuse disorders, depression, and anxiety. Their widespread occurrence across most of the world is therefore presenting serious challenges to people, communities, and health systems.
This calls for a major intervention in the areas of integration into primary health care systems, access expansion, and stigma reduction. This will mean launching public awareness campaigns, educating the public, and having open conversations about mental health in order to change the way that people in society view these services and make it easier for those who need them to get the care they need. By incorporating mental health into the process of early detection and intervention, it ensures better care coordination and more thorough treatment. Some of the root causes of mental health problems can be lessened by recognizing and addressing the social determinants of mental health, such as poverty, inequality, and a lack of social support.
6. Health Inequities and Access to Care

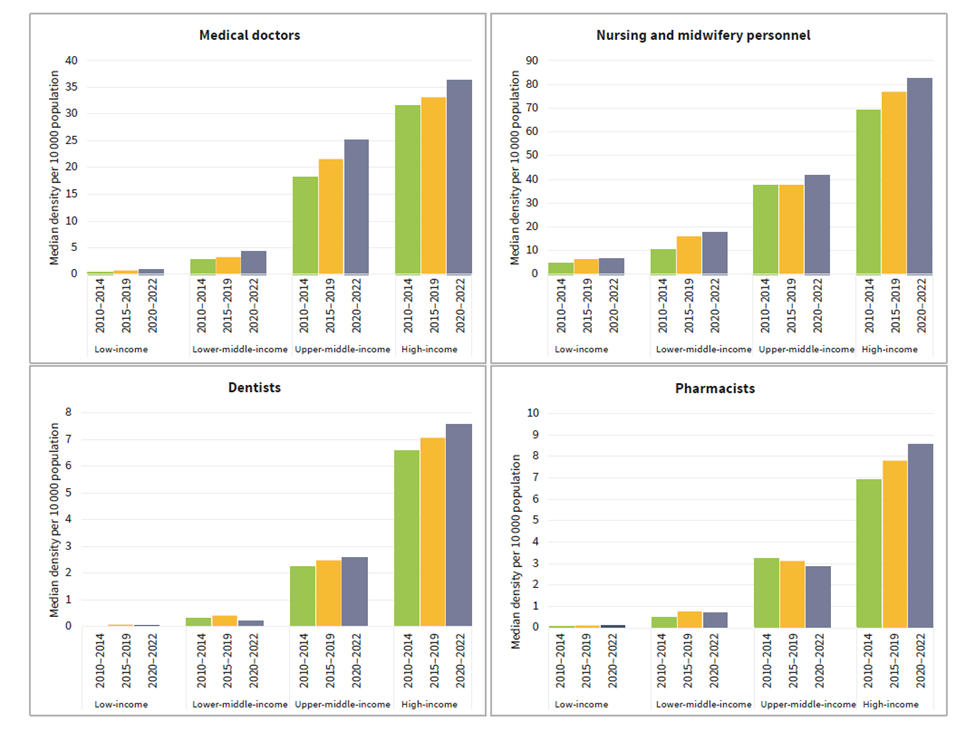
Global health disparities persist, and millions of people lack even the most basic medical interventions. At least half of the population of the world is not fully covered due to systemic injustices, geographic location, or socioeconomic reasons. Various elements fuel health disparities; these include poverty, unemployment, and illiteracy. People from the poor class tend to have high medical expenditures, underinsurance, and limited access to quality medical care. Geographical location is also another cause in areas that are usually rural or remote, few health professionals or healthcare facilities exist. Compared to Europe, which has 15.6 health workers for every 1,000 people, Sub-Saharan Africa possesses 1.3 health human resources for every 1,000 people.
What is needed to address these disparities is a multimodal response: prioritizing the health needs of the vulnerable population, investment in health infrastructure, and universal health coverage. Customized interventions like mobile health clinics, telemedicine, and community health initiatives, especially in isolated or underserved areas, play a facilitating role in closing the gaps in access to health services. Global health disparity calls for an enabling environment that will encourage international cooperation and support.
See Also: NATIONAL HEALTH PROMOTION POLICY 2019
7. Vaccine Hesitancy and Misinformation
Vaccine hesitancy, fueled by misinformation and distrust, poses a significant challenge to public health efforts in 2024. It has also been made worse by deception spread through social media platforms, leading to lower vaccination rates against diseases. For instance, measles increased by 79 percent between 2019 and 2021.
The phenomenon of vaccine hesitancy needs an integrated approach comprising community ownership, education, control of misinformation, and transparency in the processes involved in the development and distribution of vaccines. Public health campaigns for information on vaccine safety and effectiveness should be specific, factually correct, and evidence-based to address common misconceptions and concerns. Medical professionals must be involved in initiatives to engage with communities via immunization drives, health fairs, and informative workshops. Enforcing regulations against misinformation is also critical in the fight against vaccine hesitancy.

8. Food Security and Nutrition
Economic instability, conflict, and climate change have huge impacts on food security and nutrition, among many other global health concerns. In 2021, an estimated number of 768 million hungry people were recorded by the Food and Agriculture Organization in the world. These numbers are most likely to increase over the years to come. Climate change is evidenced through extreme weather events, changed temperatures, and a change in soil quality; all these factors disrupt agricultural systems and place agricultural productivity at risk.
Addressing food security and nutrition is crucial for achieving SDG 2 (Zero Hunger) and SDG 3, which include targets for ending all forms of malnutrition and ensuring access to safe, nutritious, and sufficient food for all. The WHO’s Triple Billion strategy supports efforts to improve nutrition and food security as part of its broader goal of ensuring better health and well-being for one billion more people.

9. Resilience of the Healthcare System
The COVID-19 pandemic showed why strengthening the resilience of health systems and preparation for future potential emergencies is a top priority in 2024. The development of resilience involves enhancing supply chain management, health infrastructure enhancement, and adequate inventory of basic medical supplies. We also need to invest in healthcare workers by providing them with adequate personal protective equipment, mental health support, and continuous training. Equitable remuneration and working conditions guarantee a strong health workforce and the retention of competent professionals.
Copyright: World Health Organization
10. Digital Health and Data Privacy
The adoption of digital health technologies-such as electronic health records, telemedicine, and analytics of health data-has dramatically transformed health care delivery. However, while these technologies have rendered services more efficient and hence have positively impacted patient services, they also raise considerable apprehension regarding data security, data privacy, and equality of access. Data breaches could expose sensitive personal data to discrimination and credit theft. In recognition of these fears, strict international standards for data privacy and security—including, but not limited to, laws imposing maximum protection on data through encryption, controls on access, and frequent security audits—have to be effected.

As we confront these pressing challenges that are shaping the global health landscape in 2024, we must act decisively and collaboratively. Governments, international organizations, and communities must work together to strengthen healthcare systems, invest in innovative solutions, and prioritize health equity. Taking these bold steps will foster a more resilient and healthier world for all.